The Centers for Medicare and Medicaid Services (CMS) published the final rule in the Federal Register for the fiscal year (FY) 2023 Skilled Nursing Facility Prospective Payment System (SNF PPS) on August 3, 2022. These regulations take effect October 1, 2022.
Each year, CMS publishes updates to the regulations for inflation factors, wage index adjustments, and other patient-care related payment adjustments. Below is an overview of the FY 2023 SNF PPS, including finalized changes and other relevant updates.
Key Finalized Changes
The finalized rule includes the following key changes:
- An overall finalized 2.7% increase in rates
- Wage index cap
- Code mapping classifications for the Patient Driven Payment Model (PDPM) case-mix
- Updates to the SNF Value-Based Purchasing (VBP) Program
Finalized Rate Changes
CMS updated the rates for SNFs with a net 2.7% increase. This increase included a 5.1%—or $1.7 billion—increase to payments before the recalibration adjustment is applied. The increase includes a 3.9% market basket increase, plus 1.5% to correct an error in the market basket estimate in 2021, a .3% productivity adjustment, and a 2.3% reduction for a recalibration adjustment to account for a payment increase in 2020. The net increase in payments will be approximately $904 million.
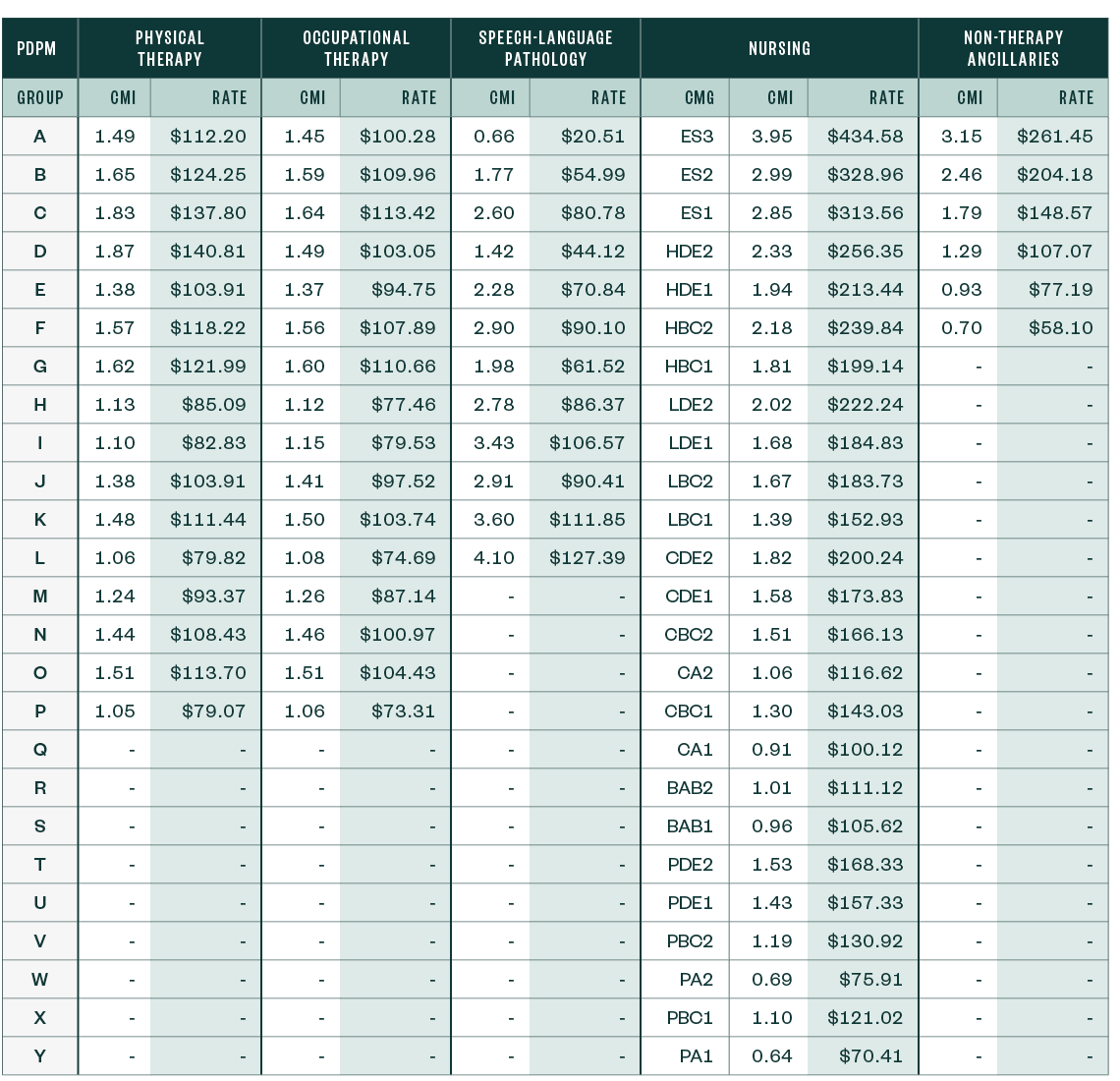
Below are the unadjusted case-mix updates for FY 2023, compared to those of the prior year, and the detailed listing of case-mix adjusted rates for FY 2023 by PDPM group.
The PDPM updates incorporate the final recalibration of the PDPM parity adjustment.
FY 2023 Unadjusted Federal Rate Per Diem—Urban

FY 2023 Unadjusted Federal Rate Per Diem—Rural

FY 2022 Unadjusted Federal Rate Per Diem—Urban

FY 2022 Unadjusted Federal Rate Per Diem—Rural

PDPM Case-Mix Adjusted Federal Rates and Associated Indexes—Urban (Including the Proposed Parity Adjustment Recalibration)
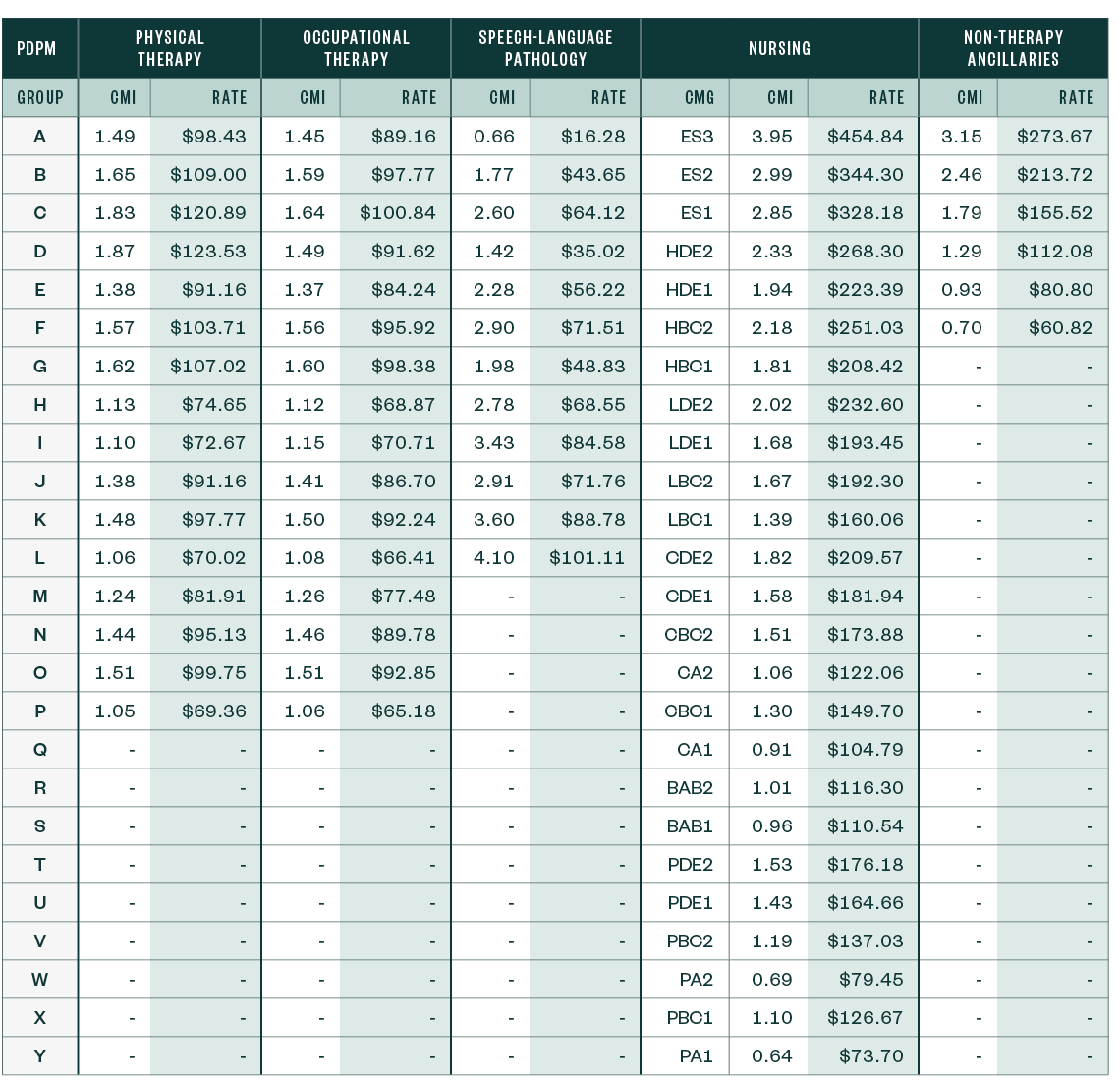
PDPM Case-Mix Adjusted Federal Rates and Associated Indexes—Rural (Including the Proposed Parity Adjustment Recalibration)
Other Notable Updates
Wage Index Cap and Core-Based Statistical Area Designation
For FY 2023, CMS finalized continuing to use the FY 2022 SNF PPS final rule that adopted the most recent Office of Management and Budget (OMB) Core-Based Statistical Area (CBSA) delineations.
However, for FY 2023 and subsequent years, CMS finalized applying a permanent 5% cap on any decreases to a provider’s wage index from its wage index in the prior year, regardless of the circumstances causing the decline.
Patient-Driven Payment Model Clinical Diagnosis Mappings
CMS finalized several changes to the PDPM ICD-10 code mappings in response to stakeholder feedback and to improve consistency between the International Classification of Diseases-10 (ICD-10) code mappings and current ICD-10 coding guidelines.
You can read the ICD-10 code mappings and lists used under PDPM.
SNF Value-Based Purchasing
Section 111 of Division CC of the Consolidated Appropriations Act, 2021, (CAA) authorizes the Department of Health and Human Services secretary to apply up to nine additional measures determined appropriate to the SNF VBP Program for payments for services furnished on or after October 1, 2023.
Due to the COVID-19 public health emergency and its effect on the readmission rates, CMS again chose to suppress the SNF 30-Day All-Clause Readmission Measure (SNFRM) from the 2023 reimbursement calculation.
Additional Provisions from CMS
CMS requested input on establishing minimum staffing requirements for long-term care facilities. While CMS received significant comments on this item, they’re still reviewing comments and will use this information for possible future rule making.
CMS finalized the adoption of a new process measure, the Influenza Vaccination Coverage among Healthcare Personnel (HCP) measure for the SNF Quality Reporting Program (QRP), beginning with the FY 2025 SNF QRP.
CMS finalized revisions to the compliance date for certain SNF QRP reporting requirements, including the Transfer of Health Information measures and certain standardized patient assessment data elements to October 1, 2023. This includes:
- Race
- Ethnicity
- Preferred language
- Health literacy
- Social isolation
CMS requested input on two future measure concepts, including:
- A functional outcome measure that includes both self-care and mobility items
- A COVID-19 vaccination coverage measure that would assess whether SNF residents were up to date on their COVID-19 vaccine
CMS received comments regarding the above and will take these comments into consideration in future rules.
Economic Impact
The overall economic impact of this final rule is an estimated $904 million in increased payments from the US federal government to SNFs during FY 2023.
This estimated impact figure doesn’t incorporate the SNF VBP reductions for certain SNFs, estimated to be $186 million in FY 2023.
Next Steps
Providers need to review whether they’ve loaded appropriate SNF rates into the patient accounting system they use to bill Medicare on or after October 1, 2022.
Once the providers incorporate the revised rates, they can validate the rates are calculated appropriately. They can accomplish this by pulling a paid claim and running it through the SNF pricer, downloadable from the CMS website.
We’re Here to Help
For more information about the final rule, possible implications for you and your organization, or assistance during your validation review, contact your Moss Adams professional.
You can also visit our Provider Reimbursement Enterprise Services page for further insights.